Newborn toxicology testing is an important identification tool. However, it is limited by testing sensitivity and timing requirements.
Overview
Why we are recommending this best practice
- The incidence of substance use in pregnancy is difficult to quantify. Maternal screening using validated surveys, and when necessary, toxicology testing in pregnancy may still underrepresent the true incidence.
- If in utero substance exposure has been identified from either prenatal history (including inquiries into prescription and nonprescription drug use) or maternal toxicology testing, this information is vital for guiding assessment and treatment options and may lead to improved outcomes for mothers and newborns.
- If maternal toxicology testing or treatment history has been confirmed, testing of the newborn may not be clinically necessary; however, it is often requested by external agencies such as child protective services (CPS). Education of CPS about the validity of other information can avoid unnecessary and in appropriate use of screening resources.
- Newborn health care providers should be provided with information on the usefulness and limitation of the birth center’s biological toxicology testing and the availability/appropriateness of confirmatory testing.
Strategies for implementation
- When the information would influence healthcare treatment, Selective biological toxicology testing should be considered for newborns when diagnostic information about the mother is limited or not available, or when the clinical picture indicates risk for in utero exposure, including but not limited to:
- Mother with limited or no prenatal care
- Maternal symptoms of drug intoxication or withdrawal that are otherwise unexplained
- Newborn signs and symptoms of potential substance exposure (i.e., withdrawal) that are otherwise unexplained
- Hospital policies and procedures should include protocols that would trigger newborn biological toxicology testing.
- Toxicology testing is limited by substance levels (concentrations) and timing. Therefore, samples should be collected and sent for analysis as soon as possible after delivery.
- Review available biological toxicology testing methods at each birth center. Traditionally, urine immunoassay has been used as the initial screen, and multiple commercial antibodies are validated.
- For certain substances, immunoassay-based urine toxicology testing is a reliable method with rapid turnaround time. For opioid exposure, routine opioid testing panels usually only detects morphine, codeine, and heroin metabolites. Synthetic opioids such as methadone, oxycodone, fentanyl, buprenorphine, etc. may require more specific testing.
- A newborn who has a biological toxicology test with unexpected positive results should have confirmatory testing (gas chromatography-mass spectrometry) and/or confirmation of drug presence by a more time specific test sample (i.e., meconium, umbilical cord).
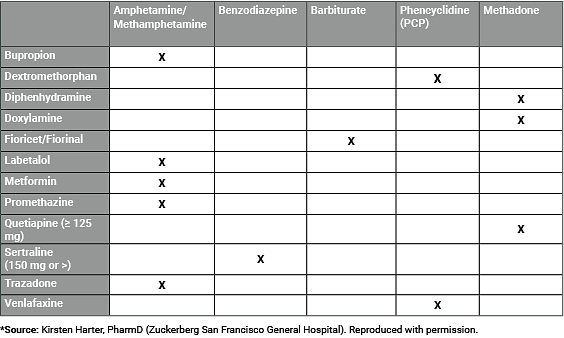
- Providers should be aware of false-positive drug testing from common maternal medications including antihistamines, antidepressants, antibiotics, decongestants, analgesics, antipsychotics, and over-the-counter products (See table below).
- Due to assay limitations, a negative biological toxicology result does not represent an absence of in utero substance exposure, specifically if the newborn exhibits clinical signs consistent with neonatal abstinences syndrome (NAS) and all other diagnoses have been appropriately ruled out.
- A positive biological toxicology result, in and of itself, does not represent child abuse or neglect. Hospitals must ensure that the multidisciplinary team caring for mothers and newborns includes social workers trained in care and treatment resources for affected families. Care should be taken to ensure that policies which delineate criteria for toxicology testing do not directly or indirectly target low income women and women of color (refer to Best Practice #3 for more information on this).
Resources
References
- Hudak ML, Tan RC. Neonatal drug withdrawal. Pediatrics. 2012; 129(2): e540- 560. doi: https://doi.org/10.1542/peds.2011-3212.
- Committee opinion no. 633: alcohol abuse and other substance use disorders: ethical issues in obstetric and gynecologic practice. Obstet Gynecol. 2015; 125(6): 1529-1537. doi: 10.1097/01.AOG.0000466371.86393.9b.
- Worley J. Identification and management of prescription drug abuse in pregnancy. J Perinat Neonatal Nurs. 2014; 28(3): 196-203. doi: 10.1097/JPN.0000000000000039.
- Bogen DL, Whalen BL, Kair LR, Vining M, King BA. Wide variation found in care of opioid-exposed newborns. Acad Pediatr. 2017; 17(4): 374-380. doi: 10.1016/j.acap.2016.10.003.
- Price HR, Collier AC, Wright TE. Screening pregnant women and their neonates for illicit drug use: consideration of the integrated technical, medical, ethical, legal, and social issues. Front Pharmacol. 2018; 9:961. doi: 10.3389/fphar.2018.00961.
- Yee LM, Wu D. False-positive amphetamine toxicology screen results in three pregnant women using labetalol. Obstet Gynecol. 2011; 117(2 Pt 2): 503-506.