Even when there is great enthusiasm around starting a quality improvement project, getting to the the goal(s) is hard without a specific plan in place. A step-by-step strategic approach or blueprint for project implementation will ensure the best possibility for success. This document is designed to guide participants through the process of implementing the toolkit to improve outcomes for mothers and newborns.
Consider the Unique Collaboration Required for Implementation
The implementation of this particular toolkit may be considered to be one of a more complex nature due to the variety of stakeholders and sites involved. Collaboration between hospitals, community resources and public health is indispensable to the implementation. Mothers and newborns affected by OUD will receive care from a diverse group of care providers. The care may well be provided in various locations outside the hospital setting. This community collaboration may add a new aspect to the hospital-focused quality improvement approach at your facility. Some facilities have a history of working closely with the community and public health. Should your facility be new to this type of collaboration, consider these partnerships as integral to success.
Education Regarding Stigma – Changing Minds
The success and sustainability of the implementation depends on the staff and provider education that takes place. While clinicians understand the importance of the right dose of the right medication, the right words are sometimes missing. "Research shows that the language we use to describe this disease can either perpetuate or overcome the stereotypes, prejudice and lack of empathy that keep people from getting the treatment they need. Scientific evidence demonstrates that this disease is caused by a variety of genetic and environmental factors, not moral weakness on the part of the individual. Our language should reflect that" (Ferner M, et al, 2017). The toolkit offers recommendations and best practices for education on stigma and substance use disorder.
Build the Right Team to Support Your Case for the Implementation Effort
Champions have the ability to communicate broadly regarding the importance of implementation, and to gain consensus for the effort. Recruit both physician and staff champions who can promote education, facilitate the implementation of the best practices and encourage others to become engaged.
The team should include those with clinical and technical knowledge, those who deal with the day to day functioning of the unit or department, and those at a higher management level with the ability to remove barriers to implementation. In a clinic setting, the team might be quite small, but teams in a more complex hospital setting require broader representation. Build a team that includes members from as many of the points of care as possible. Providers, nursing, and pharmacy professionals are all essential members of the team. Anesthesiology providers must be involved to address pain management effectively. Staff with analytic and EHR expertise should optimally be involved from the start. Quality improvement facilitators/project managers can be beneficial in organizing, communicating, and introducing QI tools at appropriate times as needed. Additionally, identify members who have been successful in previous implementation projects – large or small. Central to success, however, is finding members with a passion for improving the quality of care for substance exposed mothers and newborns.
The champions and team members should be familiar with the current state of care in the hospital as well as the data related to the goals of the implementation. Transparency regarding the data is a motivator for commitment to changing practice and minds. Reviewing the data not only identifies key opportunities but is crucial in measuring progress.
The champions and team members should have a consistent story to tell that is concise and hits the meaningful points of the goals of the implementation, the project scope and general information such as timeline and milestones.
Finally, consider including a patient representative. Hospitals are increasingly seeking input from patient and family advisory councils. This input can be especially valuable in terms of identifying the current state of the patient experience, including the practice of shared decision making.
Identify All Stakeholders and Resources
Identifying stakeholders may be simplified after an assessment of all points of care and entry in your clinic or hospital. Stakeholders may also be considered in terms of flow of care, from the prenatal period through discharge, as an example. Widen your focus to include stakeholders from outside the hospital. The goals of the toolkit (keeping the dyad together, keeping the mother in treatment, and reducing rates of NAS) can only be accomplished with ongoing relationships (communication) with providers and outside resources. In the hospital environment, as an example, it may be decided that the department representative to the medical group will support the initiative to screen patients in the office settings. Perhaps the local Department of Public Health will champion patient education materials for use in and out of the hospital.
Do not forget to include the key leaders within the hospital and outpatient services who can make critical decisions for financial and other support. Reach out to those who can assist with the appropriate channels for education for both providers and staff.
Understand the Current Landscape at Your Facility
All team members and leaders should have a shared mental model of the current culture of care in the facility as well as current practice. Transparency regarding the current state will focus implementation efforts on the most valuable areas requiring change. Transparency enables the critical discussions that need to take place in order to identify the goals for the project. What is the current state of communication and work between maternal, neonatal and pediatric departments? Where are the key connections made with community providers and resources? Are there current gaps in care?
SWOT Analysis
Understanding your current environment involves knowing your internal capabilites as well as the external environment. A SWOT Analysis is one way to evaluate your current state by categorizing your culture of care according to strengths, weaknesses, opportunities, and threats. We have included an example of an analysis below.
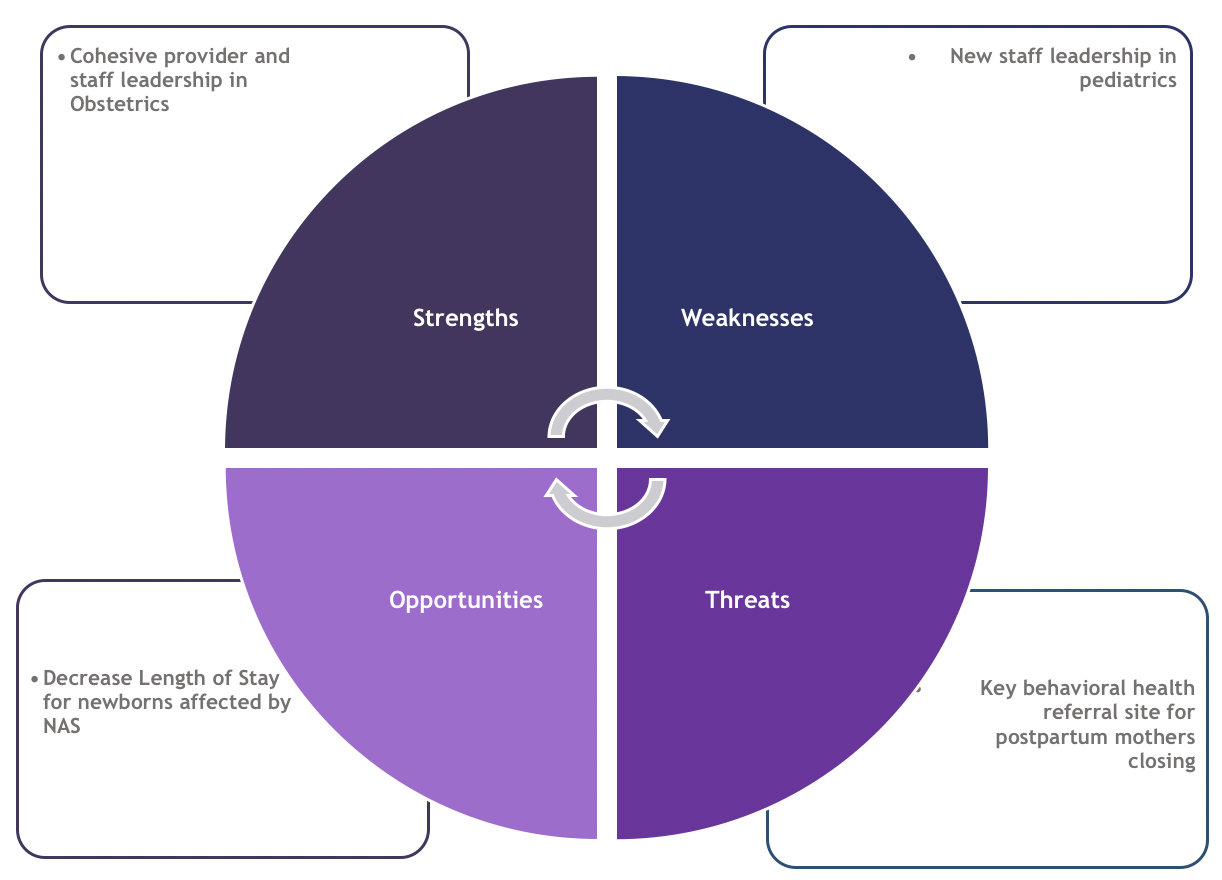
Example SWOT Analysis when considering toolkit implementation
Identify the Scope of the Project and Barriers that May Impede Progress
Scope
Identifying the scope of your project is key to success. After the team’s analysis of the current landscape at your facility, the team must make some critical decisions about which of the best practices of the toolkit should be immediately implemented. As described above, understanding the landscape of your organization, the external resources and available community services will not only illuminate what should be implemented, but also what realistically can be implemented. The scope reflects the parameters of the project – what the team will pursue and will not pursue to reach the identified goal. Just as with understanding the current landscape of care, stakeholders and the clinical champions who form the backbone of the implementation team should be included in scope planning.
Barrier Identification
Assessing barriers to implementation is also key. Many overt, general barriers to the success of the project may be easily illuminated with the SWOT or other landscape analyses described above. In this case, the barriers may be identified as weaknesses or threats. However, a more detailed, granular assessment of the barriers to the specific best practices you wish to implement will also be needed. One example of a simple brainstorming method to identify the barriers to implementing specific best practices is the “5 Whys” method. The “5 Whys” is a method of finding the root cause of why things are done a certain way (and therefore where the bottlenecks may be when trying to implement a new best practice). “By repeating why five times, the nature of the problem as well as its solution becomes clear.” In a group session, your team verbally talks through the problem you’ve identified. You ask, “why does this happen?” When you come to an answer (sometimes there is more than one answer), you ask “why does this happen” again, until you get to the actual root cause. Many brainstorming methods exist. The key is to sit down with your team and map out the possible barriers for each of the best practices you wish to implement. In the end, this methodical approach will prove impactful.
Develop Your Goals and Timeline
Based on your conversations and work to this point, develop the goals and timeline for the implementation. What are the expected outcomes? What are you really trying to accomplish? What changes can you make that will lead to improvement?
The use of SMART goals or methodology (see Resources) will move the project forward. The mnemonic is a useful tool for identifying specific, measurable, achievable, relevant, and time-bound goals. Perhaps initial project goals will revolve around self-reported screening or the identification of a template for a Plan of Safe Care. The measurable aspect may become the focus of a goal itself. Do you have a current way of measuring the percentage of patients who are screened upon admission to the hospital in labor? One of the important initial steps in designing the blueprint is to identify what you need to accomplish in the first month and then the second month and then continue to plan for every two months what specific things to accomplish. Team meetings to go over progress and strategies to overcome barriers should occur regularly. We recommend weekly or at least every two weeks at the start. Once the project is moving along, monthly meetings will likely be adequate. Research show that setting time aside from everyone’s busy schedule is an essential statement of importance and helps drive progress.
In addition, an important aspect within the timeline is the identification of milestones. Milestones note significant phases in a project, a clear sequencing of events. Reaching a milestone is also a reason to celebrate. Do not await the end of the project to celebrate – wins along the way promote cohesiveness in the team and lead to further successes.
Develop a Plan for Communication
All those involved in the implementation should be communicated with in advance of the start of the project. Utilize communication channels that have been successful in the past. There are several items to take into consideration when developing the plan:
- Would the current state of knowledge regarding the opportunity for improving outcomes for mothers and newborns affected by OUD necessitate a great deal of background information regarding the project?
- Does the comfort level of improvement efforts by staff necessitate more in-depth communication?
- Are there other ongoing improvement efforts that can be communicated with jointly in a coordinated manner?
Getting Started
It is often hard to pick which of the best practices to do first, but you can’t do them all! Different facilities will be at different stages for this project so everyone will have a different list. However, the following is a place to begin for those that are starting from scratch.
- Identify multidisciplinary project team and schedule regular meetings
- Include community partners
- Provide staff education for OUD and stigma
- Develop education and strategies for implementation of universal screening for Substance Use Disorder (including OUD)
- Establish working groups to address discharge plans (and checklists) for mothers and newborns
Resources
- California Maternal Quality Care Collaborative
- California Perinatal Quality Care Collaborative
- The History and Evolution of Smart Goals
- Institute for Health Care Improvement
- Institute for Health Care Improvement – Physician Engagement
- U.S. Department of Health and Human Services Health Resources and Services Administration: Quality Improvement
References
- Ferner, M. Here's one simple way we can change the conversation about drug abuse. The Huffington Post. December 7, 2017. https://www.huffpost.com/entry/drug-addiction-language_n_6773246. Accessed June 20, 2019.
- Fischer F, Lange K, Klose K, Greiner W, Kraemer A. Barriers and strategies in guideline implementation-A scoping review. Healthcare (Basel). 2016;4(3):36. doi:10.3390/healthcare4030036
- Seiter, C. The 5 whys process we use to understand the root of any problem. https://open.buffer.com/5-whys-process/. Accessed June 20, 2019.